Tag: Healthcare
COVID-19 has put healthcare facilities under extraordinary pressure to accomplish more with less. Nurses and doctors had to care for waves of sick patients with limited resources. Medical personnel simply didn’t have the equipment or facilities needed to keep up with patient demand, and they struggled to contain the virus with makeshift solutions.
The most obvious way to protect patients and staff from those infected with COVID-19, or any other infectious disease, is to isolate them. Proper isolation rooms have dedicated HVAC and HEPA filtration capabilities. These rooms are constructed according to stringent guidelines from the CDC and other professional associations. Isolation rooms don’t share air or controls with the rest of the medical facility to prevent the risk of cross-contamination. However, at the height of the pandemic, even the most advanced, well-funded institutions could not isolate their contagious patients.
Protecting Patients and Staff
Negative Pressure
The most common type of isolation room utilizes negative pressure. These spaces have lower pressure inside the room than in the surrounding environment. As a result, contaminants can’t sneak out of the room and spread to the rest of the hospital. A negative pressure environment is maintained by using a dedicated HVAC system that continuously pumps clean air into the room near the floor and filters and sucks it back out through a grill near the ceiling. Other patients and medical staff are protected from the sick person.
Positive Pressure
Positive pressure rooms maintain higher pressure inside a space than the surrounding environment. These rooms are connected to a hospital HVAC system, which pumps clean, filtered air into the room. When the door to the space is opened, the high pressure forces out clean air and prevents any contaminants from entering the area. Positive pressure rooms are valuable for compromised patients—burn victims, surgery patients, birthing women, and injured emergency room patients—highly susceptible to infection or pathogens.
Financial Solvency
Perhaps now more than ever, building isolation spaces dedicated to protecting and treating vulnerable patients is a prohibitively expensive option for most hospitals.
Between forced facilities shutdowns and increased costs surrounding COVID-19 preparedness, U.S. hospitals lost an estimated $323 billion in 2020. Moreover, hospitals and health systems are projected to lose between $53 to $122 billion more in 2021. Beyond shrinking budgets, administrators can be slow to adopt change due to protracted stakeholder approval processes. The path of least resistance is often to maintain the status quo.
Versatility for Enhanced Level of Patient Care
Air Innovations strives to truly understand the challenges our customers and potential clients grapple with beyond controlling temperature and humidity. Adopting a holistic approach enables us to engineer lasting solutions that are adaptable to meet their evolving needs.
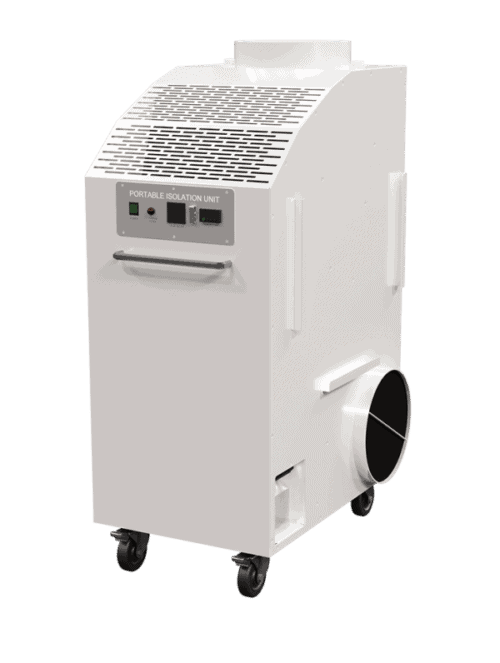
We designed the IsolationAir® system so that hospitals, medical facilities, emergency preparedness centers, and other facilities could continue delivering high-quality care to their most vulnerable patients without taking on a renovation project. Our systems convert standard-sized patient rooms into positive or negative pressure spaces depending on demand. Since the unit is portable, it limits the need for stakeholder approval often required for renovation projects. IsolationAir contamination control units are considered devices and not intrinsic parts of a hospital.
HEPA Filtration & UV Light
The portable unit includes medical-grade HEPA filtration to remove potentially harmful particles from a negative pressure space or into a positive pressure patient room. The unit also has UV-C light to sterilize internal contaminants.
Designed for Patient Comfort
IsolationAir systems have onboard heating and cooling to keep patients comfortable when they are cut off from the hospital HVAC system. The AC functionality also serves to dehumidify exam and patient rooms.
Installation Options
Each unit comes equipped with flexible ductwork, and there are two ways to implement them.
To boost readiness to respond to increased patient volumes, hospitals can pre-facilitate inpatient or exam rooms by having a universal grill adapter connected to the return grill in the ceiling. At that time, maintenance staff can check for other air exhausts or leaks in the room and seal them up. When it becomes necessary to expand surge capacity for any reason, hospital staff can rapidly deploy an IsolationAir unit by simply plugging the unit into an emergency outlet and connecting the flexible ductwork to the available adapter.
Alternatively, medical facilities can simply wheel an IsolationAir unit into a particular exam or treatment room and install a return grill adapter to which the flexible ductwork on the unit will connect. Maintenance teams can seal up visible air leaks around windows and doors. Once on-site, the process takes less than an hour and doesn’t require specialty HVAC professionals. Installing a return grill adapter as needed before connecting the unit’s ductwork is a viable option when hospitals can foresee a rise in patient demand, as we did with COVID-19.
When Flexibility Matters Most
Anytime a room is used to “open up” patients, they are immediately susceptible to potentially life-threatening pathogens. Dedicated surgical theaters are typically designed as positive pressure rooms. However, there have been instances where hospitals have opted to permanently convert surgical spaces from positive rooms to negative rooms, a transition that requires planning and time.
Trauma patients and burn victims have the best chance of survival when treated in positive pressure rooms. Issues arise when a crisis happens, and hospitals don’t have enough positive pressure rooms to treat victims. The flexibility to transform an unpressurized room into a positive pressure space quickly enables a medical establishment to treat and save more patients.
Surprisingly enough, most labor and delivery floors and emergency units don’t have contamination control even though these patients are vulnerable to infections. Often, it is impossible to anticipate whether rooms should be positive or negative pressured spaces. Hospitals, extended care facilities, and emergency preparedness centers need the flexibility to determine—sometimes on the fly—whether patients need positive or negative pressure to save their lives or to prevent catastrophe.
The Final Verdict
Despite the enormous challenges and constraints facing hospitals today, administrators have solutions available to help them respond with agility to varying patient needs. We are proud our IsolationAir system can help medical professionals do their jobs easier and enable them to save more lives. When it comes to creating spaces to care for our most vulnerable patients, versatility is the name of the game.
For Reference:
IsolationAir® Systems meet the following industry guidelines:
- 12 air changes per hour via HEPA filters
- Each IsolationAir unit conditions rooms up to 375 sq ft with an 8’ ceiling
- A pressure differential of 0.01” minimum between a room and adjoining spaces
(May require additional seals around doors or other significant leak points in large rooms with poorly sealed doors). - Continuous operation when plugged into an emergency generator outlet
- Provides stable temperature control for patient comfort
- Originally designed to meet the U.S. Department of Health and Human Services’ critical benchmarks:
- Critical Benchmark #2-2: Surge Capacity: Isolation Capacity
- Critical Benchmark #2-9: Surge Capacity: Trauma and Burn Care
- Cross-cutting Critical Benchmark #6: Preparedness for Pandemic Influenza
For additional information, see these websites:
- Centers for Disease Control and Prevention (CDC) – Guidelines for infectious disease control in health care facilities
- The American Institute of Architects (AIA) – Guidelines for design and construction of hospitals, including heating and cooling control to 75°F.
- American Society of Heating, Refrigerating and Air-Conditioning Engineers (ASHRAE) – Chapter 7 in Applications Handbook regarding health care facilities.
Note: The IsolationAir unit is an air filtration device and does not sterilize or disinfect a room or any of its contents. It is not a medical device and makes no claims for patient or healthcare outcomes. It is not intended for use in the diagnosis of disease or other conditions or in the cure, mitigation, treatment, or prevention, of disease in humans or in other animals.